Abstract
Background
The clinical course of diffuse large B-cell lymphoma (DLBCL) is variable. Although the prognostic markers and models have been developed and adapted in DLBCL, prognostic indices in relapse and refractory (r/r) DLBCL remain unclear. In order to better guide clinical practice, this study aimed to develop a prognostic nomogram in r/r DLBCL.
Patients and methods
Among 1858 DLBCL patients treated in National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital in China, between 2006 and 2016, 682 were r/r DLBCL, of which 573 patients were treated with enough cycles of first-line anthracycline-based chemotherapy. The clinical data were reviewed and evaluated. Progression free survival (PFS) was defined as the time from first treatment administration to disease progression/relapse. Relapse was defined as progression after initial complete or partial remission, and refractory disease was defined as achieving less than a partial response in the first-line setting. Cell of origin (COO) was assessed at diagnosis via Hans algorithm. The concordance index (C-index) and a calibration curve were used to determine and compare their predictive and discriminatory capacity.
Results
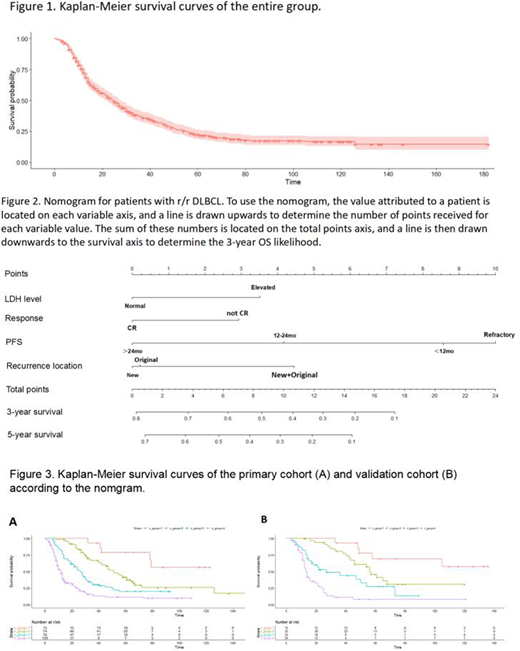
Overall, the median age at diagnosis was 54 (range 10-91) years old. Among all the patients, 325 (56.7%) were male and 248 (43.3%) were female. There were 255 (45.1%) patients categorized as stage I-II and 310 (54.9%) categorized as stage III-IV at diagnosis. Of all the patients, 145 (27.0%) were germinal center B-cell-like (GCB) and 393 (73.0%) were non-GCB. According to the Eastern Cooperative Oncology Group (ECOG) performance status (PS) score, the majority of patients had a good performance, with 457 (79.8%) of cases presenting with an ECOG PS score of 0-1; 89 (15.5%) presenting with ECOG PS of 2; 27(4.7%) scored ≥3. In the entire group, 563 (98.3%) patients received CHOP or CHOP-like regimen and 301 (52.5%) received rituximab treatment in the first-line setting. There were 200 patients (34.9%) had refractory disease; 203 (35.4%) had relapse in the first year from treatment commence; 91 (15.9%) had relapse in the second year; and 79 (13.8%) had relapse after the first 2 years. The median overall survival (OS) from diagnosis were 12, 17, 46 and 66 months, respectively in the above four groups, and OS in the entire group was shown in Figure 1. A total of 437 patients with complete clinical information were further divided into the primary (n=300) and validation (n=137) cohorts. Based on a multivariate analysis of the primary cohort, four independent prognostic factors including lactate dehydrogenase (LDH) level at diagnosis; response to the first-line treatment (CR with not CR); progression free survival and recurrence location (original with new with both) were identified and entered the nomogram (Figure 2). The calibration curve showed the optimal agreement between nomogram prediction and actual observation. In addition, the C-index of the nomogram for OS prediction was 0.743. The area under the receiver operating characteristic (ROC) curve (AUC) was 0.75 in the internal validation and 0.84 in the external validation. Four risk groups depending the nomogram were further developed and OS were presented in Figure 3.
Conclusions
Independent predictors of survival in r/r DLBCL have been identified and 4 indicators were used to create a nomogram. This proposed nomogram help with assess individual risks and decide on second-line treatment in clinical practice.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal